By Amye Anderson
UCBJ Managing Editor
JAMESTOWN – It was a Sunday like any other. Kay Price had just left church following a morning worshipping alongside her family. Opting to get her grocery shopping done on her way home, Kay decided to swing by the grocery store.
Those are a few of the last memories she has prior to waking up in the cardiovascular intensive care unit at Cookeville Regional Medical Center one week later.
Moments after pulling into the grocery store parking lot, Kay called her granddaughter, Mikayla, complaining of chest pains and stating she did not feel well. Mikayla took Price to Jamestown Regional Medical Center.
“My mother-in-law is such a character,” Sherrie Price told the UCBJ. “She walks into the Emergency Room and she stops at the desk and told the ladies there at the desk, ‘My chest is hurting, I need to see a doctor, and I don’t have time to fill out any of that paperwork.’”
There, doctors diagnosed Price with a 100-percent blockage of the left anterior descending (LAD) artery – the “widowmaker.” The LAD, a particularly important blood vessel, supplies a significant amount of blood flow to the heart muscle. Lifestyle and genetic factors can lead to a blockage of that artery over time. As cholesterol and plaque come into contact with the bloodstream, a patient could go from a minute blockage to a completely blocked artery almost instantly, meaning it could cause a massive heart attack that will lead to sudden death.
With the helicopter at least 45 minutes away, the next fastest option was to transport Kay to Cookeville via ambulance. As she lay in a unit of the emergency department at JRMC awaiting the ambulance, family members began to pour into to the waiting area. While speaking with her youngest son Kay, who had been awake and alert since arriving at the hospital, crashed.
Despite having sought medical attention almost immediately following the onset of symptoms, Kay Price, by all accounts, died in the emergency room that day.
On-call doctors frantically administered multiple shocks, at least nine doses of epinephrine, and chest massages. But, it was too late. Following approximately half an hour of attempting to revive Price, doctors requested permission to cease resuscitation efforts.
“(The doctor) said, ‘there’s no heartbeat; she’s gone,” Sherrie recalled. “They really did everything they could.”
It was after doctors pronounced Kay as being deceased that Sherrie began to carefully remove Kay’s jewelry when something almost too impossible to seem real occurred.
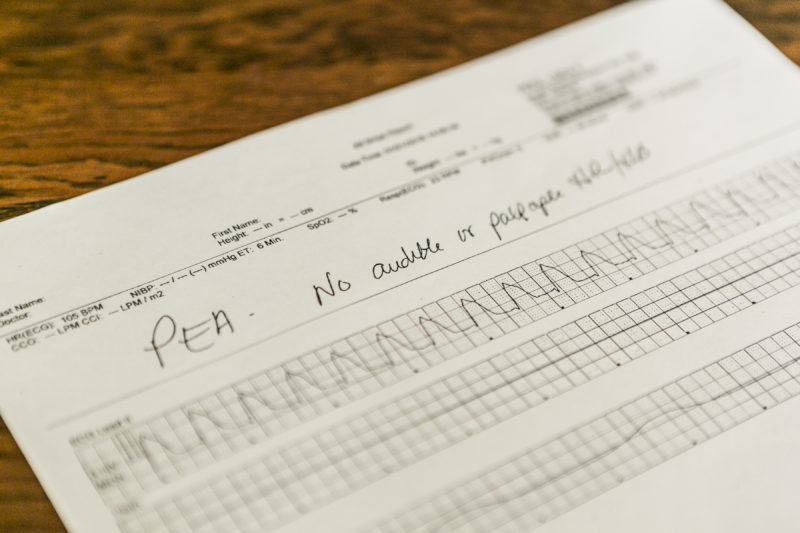
Kay’s breathing, thought to be simply a reflex known as agonal breathing, continued. After several moments of this continued breathing, a hard chest rub was performed by the doctor and a nurse was able to find a pulse.
“It was just amazing to witness,” Sherrie told the UCBJ. “It was unbelievable.”
Dr. Charlie Fang, the physician who cared for Kay during her stay at JRMC, reportedly told the family what Kay experienced was a miracle.
“A little bit later, I guess when they were about to load her into the ambulance, Dr. Fang was there with all of the family and we were all there talking and he looked at my husband and said, ‘This is why we pray,’” Sherrie recalled.
Kay was then transported to Cookeville for further treatment. Doctors there diagnosed a 100-percent blockage and Dr. Matthew Sample placed a stent inside the artery to improve circulation and blood flow. Doctors then determined Kay was a good candidate for hypothermia treatment.
But, with Kay unconscious, and her brain having been without sufficient oxygen, from the time resuscitation efforts were ceased and a pulse detected, doctors weren’t immediately able to determine the extent of the brain damage, if any.
Hypothermia therapy, reducing the body’s core temperature down to about 90 degrees, is shown to have positive effects on patients who have experienced cardiac episodes in which the brain and other organs have been oxygen-starved for longer periods of time. Inducing a hibernation-like state, further brain damage can be reduced, depending on timing.
After 24 hours, Kay’s core temperature was slowly increased. Days later, Kay came to with no memory of the events of the previous days.
“She doesn’t remember anything,” Sherrie said. “She remembers being at church on Sunday before it happened but she doesn’t remember leaving church, she doesn’t remember driving to the grocery store, she doesn’t remember calling Mikayla or even going to the Jamestown ER.”
She was back home one week later and stayed with Sherrie and her husband, Kay’s oldest son, Stacy, while she progressed through a few weeks of physical therapy.
In Kay’s case, she doesn’t recall feeling unwell – tired, short of breath, nauseous or any of the other so-called classic signs and symptoms of a heart attack; not an uncommon occurrence.
Kay, who mows lawns for the living, was active leading up to the heart attack.
“(She’s) very active, could outwork most men half her age. She’s such a hard worker,” Sherrie said.
However, Kay’s father experienced a fatal heart attack in his late 50s and she speculates her risk was higher due to genetic factors.
CRMC cardiologists recommend seeking medical treatment right away if the following symptoms are experienced:
- Discomfort in center of chest lasting more than a few minutes, or pain that goes away and returns; uncomfortable pressure, squeezing, fullness, or pain.
- Discomfort in other areas of the upper body.
- Pain or discomfort in one or both arms, the back, neck, jaw or stomach.
- Shortness of breath can also occur with or without discomfort.
The Heart and Vascular Center at CRMC is the only level-three accredited chest pain center in the Upper Cumberland awarded the Society of Chest Pain Centers. Since 1994, approximately 31,000 heart catheterizations have been performed, along with more than 4,100 open heart surgeries; along with a full range of other cardiac and vascular procedures and services.
Every 40 seconds, someone in the United States has a heart attack – approximately 790,000 Americans annually – according to the Centers for Disease Control. Of these, 580,000 are experiencing a heart attack for the first time.









